
Retinal Detachment 101
January 30, 2020

Most people know someone who has suffered from a detached retina. You might think it will never happen to you, but it is still very important to know the signs and symptoms. The best outcomes come from urgent treatment, so it is crucial to act quickly if you think you might have a retinal detachment.
What is a retinal detachment?
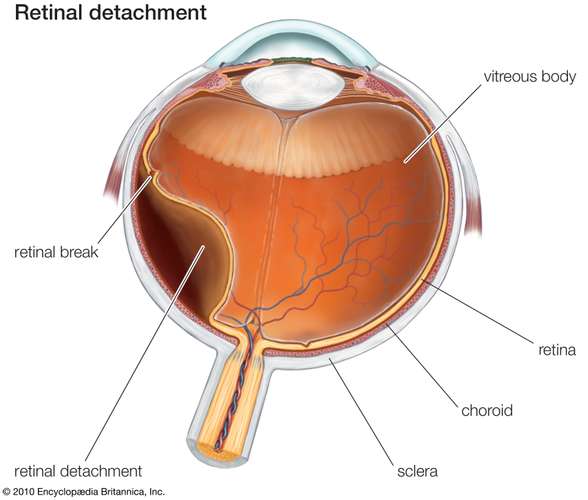
The retina is a very thin layer of tissue that lines the inside of the eyeball. This specialized nerve tissue is an important part of the visual pathway.
When a person experiences a retinal detachment, the retina separates from the back of the eye, which contains the necessary supply of nutrients and connections to the brain for processing vision. If the retina is not reattached to the back of the eye in a prompt manner, permanent vision loss occurs.
What are the symptoms of a retinal detachment?
There is no pain associated with a retinal detachment, so you cannot actually feel the retina detaching. The following are the most common symptoms of a retinal detachment:
- Sudden or worsening floaters
- Flashes of light in vision
- Curtain-like shadow, darkness, or blur that gradually moves across field of view
- Blurred vision
What are the causes of a retinal detachment?
There are three main causes of a retinal detachment:
- Rhegmatogenous: A hole or tear in the retina allows fluid to get under the retina, which causes the detachment. This is the most common type and is usually associated with the aging process that occurs to the vitreous gel in the eye.
- Tractional: Retinal scar tissue pulls on the retina causing the detachment. This is usually seen in people with poorly controlled diabetes.
- Exudative: Fluid builds up under the retina and pushes the retina away from the back of the eye. There are no tears or holes associated with an exudative detachment. This is more commonly seen in people with age-related macular degeneration, an eye tumor, or eye injury.
What are the risk factors of a retinal detachment?
Although anyone can have a retinal detachment, the following conditions increase the risk of a retinal detachment:
- High myopia (nearsightedness)
- Older age
- Family history of retinal detachment
- Previous retinal detachment
- Posterior vitreous detachment (gel in the center of the eye pulls away from the retina)
- Recent eye injury or surgery
- Other eye diseases: uveitis (ocular inflammation), lattice degeneration (thinning of retina), diabetic retinopathy
How is a retinal detachment diagnosed?
If any of the previously listed symptoms are present, call an eye doctor immediately.
A dilated eye exam is the best way to detect a retinal detachment because it exposes the entire retina into view. Macula scans are also helpful if the detachment is affecting the central vision. If there is an obstruction blocking the view, such as a cataract, an ultrasound scan can be used to grossly view a detachment.
What is the treatment for a retinal detachment?
Surgery is typically the treatment for a retinal detachment, however, there are different methods based on the location and severity of the detachment. Usually a combination of these procedures is utilized.
- Pneumatic retinopexy: A gas bubble is injected into the vitreous gel, which pushes against the retinal detachment when the head/body is positioned accordingly. This surgery requires the patient to keep a specific head posture for several days.
- Vitrectomy: The vitreous gel in the eye is removed and replaced with a silicone oil or gas bubble to push the retina back onto the underlying tissues. Similarly to pneumatic retinopexy, a specific head position may be required.
- Scleral buckle: A silicone “belt” or band is sewed around the eyeball to indent the eye. This pushes the outer part of the eye closer to the detachment and helps reposition the retina back into place. The buckle is not visible after surgery. Any fluid below the retina is also removed.
- Cryopexy: A freezing probe is applied to the outer part of the eye to induce scar formation that helps the retina adhere back to the eyeball.
- Laser procedure: This spot-treats focal areas to seal the retina back to its normal position. It can also be used as a “barrier” to protect the retinal tear or hole from spreading to a larger area.
If let untreated, a retinal detachment results in permanent vision loss. Even with treatment, there is still a risk of permanent vision loss, especially the longer it has been present without treatment. One of the best predictors of post-operative vision is the amount of vision loss prior to surgery.
There is really no way to prevent a retinal detachment besides wearing protective eyewear for sports; However, an annual comprehensive exam can help detect early signs that may indicate risk of a future detachment. Call to schedule your appointment today!