
The Big 3: Cataracts + Glaucoma + Macular Degeneration
January 26, 2023
“My grandma had glaucoma. No, it was cataracts. Maybe it was macular degeneration. What’s the difference?”
When we ask if there is any family history of eye problems, these are the big ones that we hear most frequently, but they are also some of the most misunderstood conditions too. This blog will summarize key facts regarding the BIG 3 ocular conditions – cataracts, glaucoma, and macular degeneration.
Cataracts

Everyone will develop cataracts at some point later in life, so it is important to understand what can be expected. We are born with a crystal clear lens that sits behind the iris in each eye. Over time, the lens begins to turn yellow or hazy, which is typically the result of UV light exposure, medications, and other lifestyle factors (smoking, radiation, trauma, genetics, systemic diseases, nutrition) that alter the lens proteins. These changes cause the lens to harden, rather than remaining flexible and malleable. This is called nuclear sclerosis, which literally translates into hardening of the nucleus (the centermost part of the lens).
Yellowing of the lens is usually apparent by the time people are in their 60s, however, vision changes may take years to notice. The average age for cataract surgery in the United States is 73 years old. Since cataract surgery has been greatly refined over the last 20 years, it seems that people are not waiting as long to have cataract surgery anymore. If there are vision complaints associated with the presence of cataracts, then the issue is addressed rather than waiting until the vision is severely compromised.
There is no proven method to prevent cataracts, as they are part of the natural aging process that occurs to everyone’s eyes. Avoiding smoking, wearing sun protection, and eating a healthy diet are all positive lifestyle factors that can possibly delay the onset and progression of cataracts, but it is impossible to truly stop the formation of cataracts.
Glaucoma
Glaucoma is a chronic, progressive condition that causes damage to the optic nerve. The optic nerve is a “cable” of approximately 1 million individual nerve fibers that connect the eye to the brain. Continually increased eye pressure causes damage to the optic nerve. The nerve fibers responsible for peripheral vision are typically the first to become damaged, which correlates to permanent loss of peripheral vision. Blindness is possible in advanced or severe forms of glaucoma.
Although anyone can have glaucoma, there are several risk factors that increase the chances of developing glaucoma. Those at a higher risk include people with a family history of glaucoma, age of 60+ years old, poor circulation (could be due to diabetes, migraines, or sleep apnea), and history of eye trauma.
The scary thing about glaucoma is that there are little to no symptoms, which makes it nearly impossible to diagnose without a comprehensive eye exam.
Glaucoma is diagnosed during a comprehensive eye exam with supplemental testing. Eye pressure and optic nerve appearance are both important factors in detecting glaucoma. Optic nerve scans, using an OCT, and visual field testing are extremely helpful in monitoring the disease progression. Although there is no cure for glaucoma, decreasing the eye pressure can slow the progression to minimize vision loss. This is usually accomplished using prescription pressure-lowering eye drops.
Age-Related Macular Degeneration
Age-related macular degeneration (AMD) is a condition that affects the part of the retina responsible for central vision. The accumulation of retinal waste products, or drusen, causes progressive damage and leads to permanent atrophy of the macula. Abnormal blood vessels can also grow and leak into the retina, which causes swelling and toxic damage to the macula. The presence of blood and/or fluid in the retina differentiates the “wet”, or neovascular, form of AMD from the “dry” type.
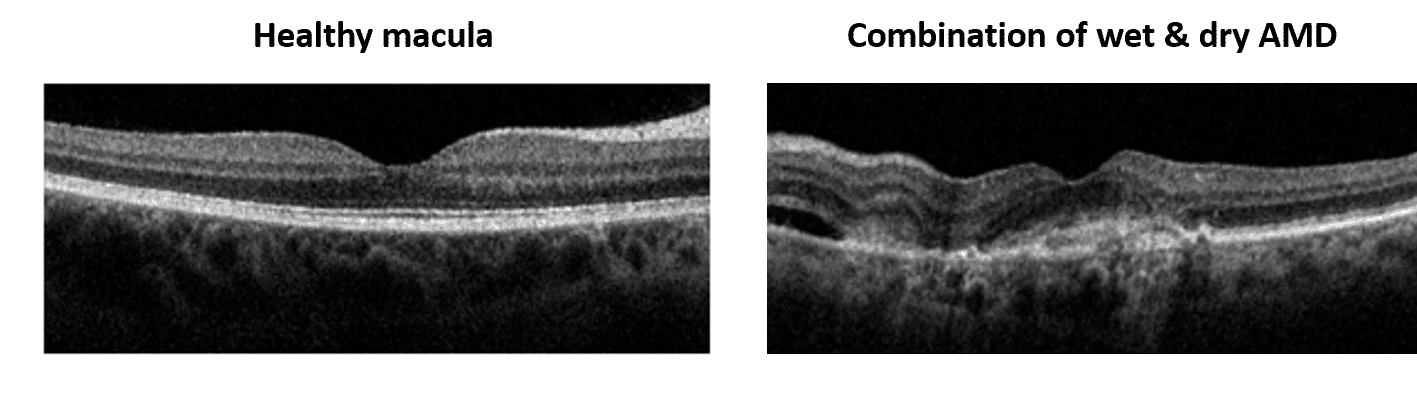
The first symptom is usually blurred vision, and straight lines may appear wavy or distorted. As the condition progresses, central vision can be completely lost as if there is a dark or missing spot in the center of vision. While the biggest risk factor is age, other notable risk factors include smoking cigarettes, family history of AMD, and light-colored eyes.
There is no treatment for dry AMD, however, the Age-Related Eye Disease Studies (AREDS) have shown that a special formulation of vitamins and minerals can slow the progression of dry AMD once in the intermediate disease stage. The most common form of treatment for wet AMD is a series of medicated injections in to the eye. The medicine blocks the growth of new blood vessels in hopes of decreasing the amount of bleeding and fluid under the retina. If vision loss progresses even with treatment, there are low vision services are available for teaching ways to cope and function with decreased vision.
Hopefully this summary is helpful in explaining the basic differences between the BIG 3 common conditions – cataracts, glaucoma, and macular degeneration.