
What is an Epiretinal Membrane?
July 8, 2022
An epiretinal membrane goes by several names – ERM, cellophane maculopathy, and macular pucker. It consists of semi-clear, fibrocellular material that grows into a membrane on the surface of the retina in the macula region. Most people know of the macula in association with age-related macular degeneration. ERMs are usually unilateral, or occurring only in one eye; However, it can happen in both eyes.
What causes an epiretinal membrane?
The vitreous, or gel-like substance inside the eye, is firmly attached to the retina at birth. Over time, the vitreous begins to liquefy in adulthood, which causes it to shrink and slowly pull away from the retina. It is suspected that this natural, aging process can initiate the start of an ERM in some individuals. Most ERMs are idiopathic, meaning the cause of the problem is unknown.
During a posterior vitreous detachment, there is a greater risk for an ERM due to the traction between the vitreous and the retina. Once the vitreous has completely separated from the macula, the ERM usually remains fairly stable. In rare cases, the vitreous can pull the membrane off of the retina, which results in spontaneous resolution of the ERM.
Retinal surgeries to repair a hole, tear, or detachment can cause traction, which leads to the formation of an ERM. Similarly, ERMs can be associated with vascular diseases of the retina (diabetic retinopathy and vein occlusion).
Who is at risk for an epiretinal membrane?
Age is one of the biggest risk factors for developing an ERM. Most people with ERMs are 50 years or older because the molecular properties of the vitreous begins to change with increasing age.
Individuals with an impending posterior vitreous detachment or vitreomacular traction (pulling at the interface of the vitreous and macula) are at a higher risk for a secondary ERM, due to its respective source.
A history of retina surgery, uncontrolled diabetes, and vein occlusion are also risk factors for developing an ERM.
What are the symptoms associated with an epiretinal membrane?
Most people do not have any symptoms with an ERM until it affects the fovea, which is the central-most part of the macula that is responsible for precise, detailed vision.
If the ERM becomes large enough, it can cause metamorphopsia, or visual distortions. Straight lines may appear wavy, and there could be a general blur in the affected eye. Some people also experience monocular double vision, which is double vision that remains present even if one eye is covered.
How is an epiretinal membrane diagnosed?
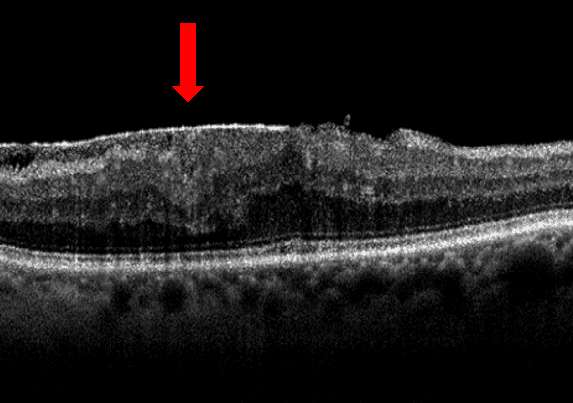
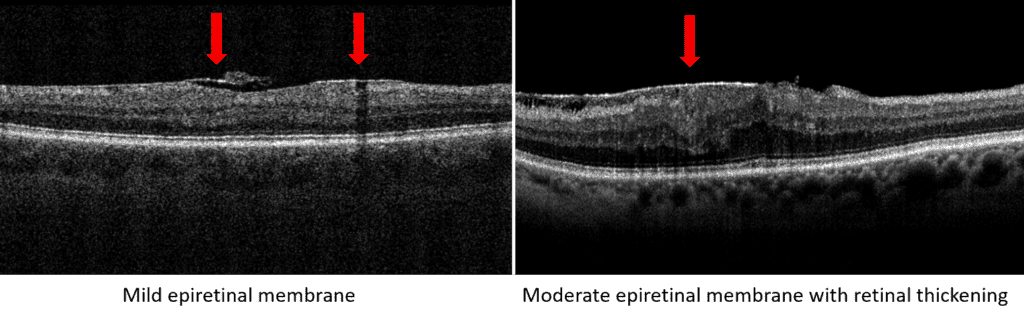
An optical coherence tomography (OCT) scan can detect the presence of an ERM, and it is a very useful tool in determining the severity. OCT scans also allow the eye care provider to monitor for changes or worsening of the membrane.
The ERM can pull on the retina, which wrinkles the most superficial layers of the retina. The pulling of the retina can cause macular thickening from all the stretching. If there is a central hole in the ERM, it mimics the appearance of a macular hole and is called a pseudohole.
ERMs can also be visualized during a dilated examination, however, it can be difficult to assess the effects on the individual retinal layer thickness without the use of an OCT.
The iWellness scan is the perfect screening tool to assist in diagnosing ERMs. This helps guide the rest of the exam and set appropriate expectations for visual outcomes. Once a baseline scan is established, there are more detailed OCT scans that can be repeated every 6 to 12 months.
What is the treatment of an epiretinal membrane?
Most ERMs are monitored for worsening and associated findings. Treatment is not performed unless there is a significant effect on vision.
If vision is severely compromised, a retina specialist can surgically remove the ERM with a vitrectomy and membrane peel. The vitreous is removed from the eye to provide better accessibility for the surgeon to delicately peel the membrane away from the retina. The vitreous is replaced with an artificial substitute, and vision should gradually improve over the course of several months. Most people will develop cataracts within a year of having a vitrectomy, and there is a higher risk for a retinal detachment.
Is there any way to prevent an epiretinal membrane?
Unfortunately, there is no way to prevent an idiopathic ERM from occurring. Controlling diabetic retinopathy and other vascular conditions can help prevent secondary ERMs. Annual eye exams are crucial in detecting both vision and ocular health changes.